TAU Discovery Decodes a Rare Neurological Disease
This breakthrough could pave the way for neurological treatments.
Researchers at Tel Aviv University have developed an innovative research model that allowed them to decode the mechanism underlying a severe and rare neurological disease. The disease is characterized by symptoms such as epilepsy, developmental delay, and intellectual disability.
According to the researchers: “Decoding the disease mechanism is a critical step toward developing treatments targeting specific cellular functions for this disease and other conditions with similar mechanisms affecting cellular energy production”.
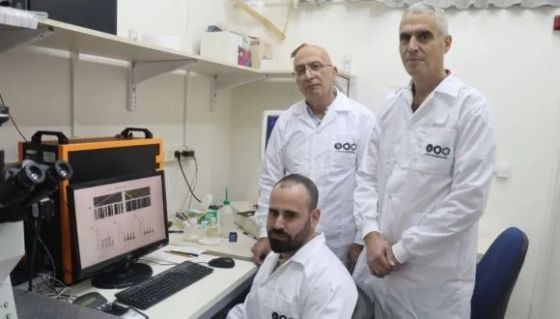
The research was led by Tel Aviv University’s Prof. Abdussalam Azem, Dean of the Wise Faculty of Life Sciences, in collaboration with Prof. Uri Ashery and PhD student Eyal Paz from the School of Neurobiology, Biochemistry and Biophysics at the Wise Faculty of Life Sciences and the Sagol School of Neuroscience. Additional contributors included Dr. Sahil Jain and Dr. Irit Gottfried from the School of Neurobiology, Biochemistry, and Biophysics at Tel Aviv University, Dr. Orna Staretz-Chacham from the Faculty of Health Sciences at Ben-Gurion University, Dr. Muhammad Mahajnah from the Technion, and researchers from Emory University in Atlanta, USA. The findings were published in the prominent journal eLife.
TIMM50 Mutation Linked to Rare Brain Disorders
Prof. Azem explains: “The disease we studied is caused by a mutation in a protein called TIMM50, which plays a crucial role in importing other proteins into the mitochondria—the organelle considered the cell’s energy powerhouse. The human mitochondria operate with about 1,500 proteins (approximately 10% of all human proteins), but only about 13 of them are produced within the mitochondria itself. The rest are imported externally through various mechanisms. In recent years, mutations in the TIMM50 protein, which is responsible for importing about 800 proteins into the mitochondria, were found to cause severe and rare neurological disease with symptoms like epilepsy, developmental delay, and intellectual disability”.
Prof. Ashery adds: “Protein import into the mitochondria has been extensively studied over the years, but how a mutation in TIMM50 affects brain cells was never tested before. To investigate this for the first time, we created an innovative model using mouse neurons that mimics the disease caused by the TIMM50 protein mutation. In this study, we significantly reduced the expression of the protein in mouse brain cells and observed its impact on the cells”.
How Does a Protein Defect Link Energy Loss to Epilepsy?
Eyal Paz explains: “The impairment of the protein led to two main findings: a reduction in energy production in the neurons, which could explain the developmental issues seen in the disease and an increase in the frequency of action potentials (the electrical signals that transmit information along neurons and enable communication between them). This increase in action potential frequency is known to be associated with epilepsy. The change in frequency is likely caused by significant damage to two proteins that function as potassium channels. Imbalances in potassium levels can lead to life-threatening conditions, such as arrhythmias, cardiac arrest, and muscle weakness, potentially leading to paralysis. These potassium channels may serve as potential targets for future drug treatments for the disease”.
Prof. Azem concludes: “Our study decodes the mechanism of a severe and rare neurological disease caused by a mutation in a protein critical for importing proteins into the mitochondria. Understanding the mechanism is a crucial step toward treatment, as it enables the development of drugs targeting the specific issues identified. Additionally, we created a new research model based on mouse neurons that significantly advances the study of protein import into mitochondria in brain cells. We believe that our findings, combined with the innovative model, will enable more in-depth research and the development of treatments for various neurological diseases caused by similar mitochondrial dysfunction mechanisms”.
