Protein Mapping Pinpoints Why Most Metastatic Melanoma Patients Do Not Respond to Immunotherapy
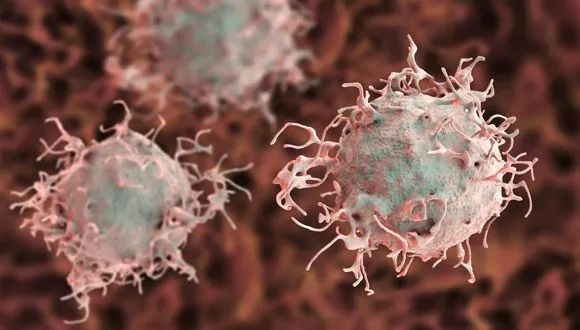
Lipid metabolism found to affect cancer cells’ visibility to the immune system, say TAU, Sheba Medical Center researchers
Tel Aviv University and Sheba Medical Center researchers say they have discovered why more than half of patients with metastatic melanoma do not respond to immunotherapy cancer treatments.
Wielding proteomics, an innovative “protein mapping” approach, a team of researchers led by Prof. Tami Geiger, Prof. Gal Markel, and Dr. Michal Harel of TAU’s Sackler School of Medicine and Sheba’s Ella Lemelbaum Institute for Immuno-Oncology have answered the burning question: Why do immunotherapy treatments greatly help some patients with melanoma but not affect 60 percent of metastatic melanoma patients?
The researchers, whose findings were published on September 5 in Cell, compared the responses of 116 melanoma patients to immunotherapy — one group in which immunotherapy was successful and a second in which immunotherapy was not successful. Harnessing proteomics, a powerful protein mapping technology, they discovered differences in the metabolism, or energy production process, of the cancer cells of the two groups.
“In recent years, a variety of cancer immunotherapy therapies have been used, therapies that strengthen the anti-cancer activity of the immune system,” explains Prof. Markel, a senior oncologist and scientific director of the Ella Lemelbaum Institute. “These treatments have been shown to be highly effective for some patients and have revolutionized oncology. However, many patients do not respond to immunotherapy, and it is critical to understand why.
“Can we predict who will respond? Can we alter treatment in order to increase responses? In our research, we focused on metastatic melanoma, a devastating disease that until recently had no efficient treatments. It was clear to us that pre-treatment samples from responders and non-responders would be key.”
To better understand treatment resistance mechanisms, the scientists examined tumors taken from 116 patients using proteomics.
“In the proteomic lab, we use an instrument called a mass-spectrometer, which enables global mapping of thousands of proteins,” explains Prof. Geiger, head of TAU’s Proteomics Lab. “We then followed up with extensive computational analysis to identify the proteins that differentiated between the response groups.”
The proteomic comparison identified major differences between responders and non-responders to immunotherapy. “In the responders, we found higher levels of proteins associated with lipid metabolism, which led to better recognition by the immune system,” says Prof. Geiger.
In collaboration with the Salk Institute in San Diego and Yale School of Medicine, researchers then examined their findings in melanoma tissue cultures and a mouse model of metastatic melanoma.
Using genetic engineering, they were able to silence the mechanism responsible for fatty acid metabolism.
“We found that upon silencing this metabolic pathway, the cancer cells manage to ‘hide’ from T-cells that are supposed to detect and destroy them,” says Prof. Geiger. “As a result, cancer in these mice developed at a faster rate compared to the control group.
“In our study, we identified a significant difference between melanoma patients who live for years thanks to immunotherapy, and patients who are not at all affected by the treatment.”
“These findings can also be relevant to many other malignancies,” adds Prof. Markel. “Now, in subsequent studies, we are looking for ways to improve the response to immunotherapy and expand the circle of patients who benefit from it. In addition, we are looking for a method that will allow clinicians to anticipate which patients will respond to treatments.”
Related posts






Destroying Cancer: new drug delivery system containing RNA therapy can target cancer cells in bone marrow





Operation Guardian of the Walls: Women, Young People and Residents of the South Paid the Heaviest Price



Breakthrough Gene Therapy Offers Hope for Severe Developmental Epilepsy in Children

Prof. Isaac P. Witz Honored with 2023 Szent-Györgyi Prize for Progress in Cancer Research