TAU Researchers Identify COVID Proteins that Cause Strokes and Heart Attacks
Findings may help develop drug to halt virus’ damage to blood vessels.
Two years into the global pandemic, we still do not know which of the proteins in the SARS-CoV-2 virus are the ones responsible for cases of severe vascular damage. For the first time since the outbreak of COVID-19, a TAU-led team of experts has been able to identify 5 of the 29 proteins that make up the virus that are responsible for damaging blood vessels. The researchers hope that the identification of these proteins will help develop targeted drugs for COVID-19 that reduce vascular damage.
Coronavirus Deconstructed
“We see a very high incidence of vascular disease and blood clotting, for example stroke and heart attack, among COVID patients,” says Dr. Ben Maoz of TAU’s Department of Biomedical Engineering and Sagol School of Neuroscience. “We tend to think of COVID as primarily a respiratory disease, but the truth is that coronavirus patients are up to three times more likely to have a stroke or heart attack. All the evidence shows that the virus severely damages the blood vessels or the endothelial cells that line the blood vessels. However, to this day the virus has been treated as one entity. We wanted to find out which proteins in the virus are responsible for this type of damage.”
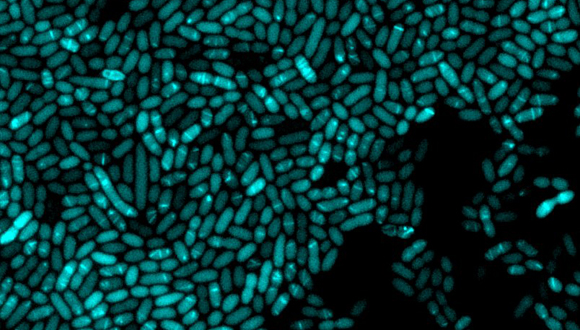
The novel coronavirus is a relatively simple virus – it comprises a total of 29 different proteins (compared to the tens of thousands of proteins produced by the human body). The Tel Aviv University researchers used the RNA of each of the COVID-19 proteins and examined the reaction that occurred when the various RNA sequences were inserted into human blood vessel cells in the lab; they were thereby able to identify five coronavirus proteins that damage the blood vessels.

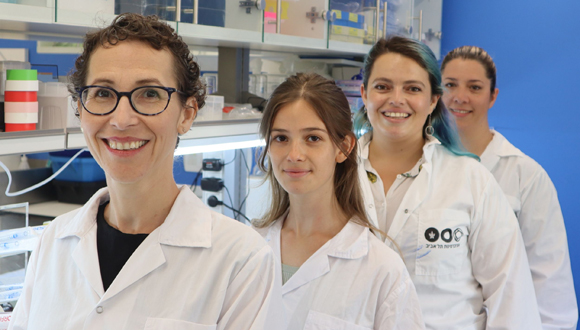
Dr. Ben Maoz in his lab
Minimizing Damage to Blood Vessels
“When the coronavirus enters the body, it begins to produce 29 proteins, a new virus is formed, that virus produces 29 new proteins, and so on,” explains Dr. Maoz. “In this process, our blood vessels turn from opaque tubes into kind of permeable nets or pieces of cloth, and in parallel there is an increase in blood clotting. We thoroughly examined the effect of each of the 29 proteins expressed by the virus, and were successful in identifying the five specific proteins that cause the greatest damage to endothelial cells and hence to vascular stability and function. In addition, we used a computational model developed by Prof. [Roded Sharan of the Blavatnik School of Computer Science] which allowed us to assess and identify which coronavirus proteins have the greatest effect on other tissues, without having seen them ‘in action’ in the lab.”
According to Dr. Maoz, the identification of these proteins may have significant consequences in the fight against the virus. “Our research could help find targets for a drug that will be used to stop the virus’s activity, or at least minimize damage to blood vessels.”
The study was led by Dr. Ben Maoz of the Department of Biomedical Engineering and Sagol School of Neuroscience, Prof. Uri Ashery of The George S. Wise Faculty of Life Sciences and Sagol School of Neuroscience, and Prof. Roded Sharan of the Blavatnik School of Computer Science – all Tel Aviv University researchers. Also participating in the study were Dr. Rossana Rauti, Dr. Yael Bardoogo and doctoral student Meishar Shahoah of Tel Aviv University, and Prof. Yaakov Nahmias of the Institute of Life Sciences at the Hebrew University. The results of the new study were published in the journal eLife.
Featured: Illustration of Coronavirus in blood vessel