- Aiding the authorities focus quarantine efforts, understand if there are “super-spreading” infected individuals, and predict how quickly the disease spreads or wanes.
- Screening Israeli COVID-19 survivors for antibodies as a basis for therapies and a vaccine.
- Developing novel inhibitors for viral entry and viral activity.
- Finding candidate compounds to kick in the body’s natural immunity to COVID-19 and ability to overcome infection.
- Understanding lung immune responses to viral infection.
- Introducing a robotic system for much faster detection of coronavirus presence in tests.
- Repurposing known and FDA-approved drugs for prevention and treatment.
Tag: Medicine
TAU Student, COVID-19 Sprint Invent Disposable Ventilators to Help Treat Coronavirus Patients
TAU Student, COVID-19 Sprint Invent Disposable Ventilators to Help Treat Coronavirus Patients
Israel’s Health Ministry has approved the use of a prototype in a pilot study Together with COVID-19 Sprint, a technology task force led by Assuta Ashdod Hospital, Rafael Advanced Technology and Weizmann Institute of Science, a doctoral student at Tel Aviv University‘s Iby and Aladar Fleischman Faculty of Engineering is helping to develop an inexpensive disposable ventilator specifically tailored to treat COVID-19 patients. It’s called MANSHEMA, is cheap, suitable for mass production and easy to use, and Israel’s Health Ministry recently approved the use of its prototype in a pilot study. “Around the world, hospitals overwhelmed with COVID-19 patients are experiencing a shortage of ventilators,” explains Stav Bar-Sheshet, a doctoral student of engineering engaged in research for the project. “This is a serious crisis, which requires creative and revolutionary thinking, thinking that will result in the efficient, fast and cheap solutions.” The idea, he says, is to produce a cheap, disposable ventilator from existing parts that are widely available. While MANSHEMA is disposable, it can work nonstop for three months at a stretch. Most critically for the novel coronavirus, the cheaply produced ventilator is tossed out after each use, drastically reducing the risk of infection by medical staff and hospital patients. “Coronary disease is highly contagious,” adds Bar-Sheshet. “The unique idea of the disposable respirator is that after being used on one patient, it will be destroyed and a new ventilator applied to a subsequent patient.” MANSHEMA is a flow driven, electronically controlled system that allows the patient to determine his or her own respiratory rate and to alert of malfunctions and respiratory failures. The system assists the patient to breath by providing what’s called Bi-level Positive Pressure, meaning the system maintains a positive pressure at all times to assist in cases of respiratory distress. Both exhalation and inhalation pressures can be adjusted by both the patient and medical staff. The system is noninvasive and particularly suited to low to moderate risk patients. “An electrically-controlled-mechanical-valve opens and closes the exhaust to allow real-time inhale and exhale,” says Bar-Sheshet. “If the patient stops breathing, alerts are triggered and the system automatically enters a mandatory respiration mode.” In a spirit of friendly competition, COVID-19 Sprint has set up two to three teams for each challenge. Each team contains a core group of builders (product manager, engineers, solution architects), with a clinical advisory group advising each challenge. Volunteers with experience as engineers, product managers, clinicians, care managers, project managers are welcome to join existing teams or create new teams. “To date, the team, with the support of the Health Ministry, have a few prototypes tested by medical staff at Assuta Ashdod Hospital,” concludes Bar-Sheshet. “The Health Ministry helped us meet Helsinki requirements that will now allow us to proceed to a clinical trial on patients with respiratory problems and on COVID-19 patients.”TAU to partner with InnoCan Pharma on revolutionary COVID-19 treatment
The technology, which is expected to be administered by inhalation, will be tested on several lung infections
InnoCan Pharma Corporation announced that its wholly-owned subsidiary, InnoCan Pharma Ltd. of Herzliya Israel, has entered into a sponsored research agreement with Ramot at Tel Aviv University to jointly develop a novel, revolutionary approach to treat COVID-19 by using cannabidiol (CBD) loaded exosomes (“CLX”). Under the terms of the Research Agreement, InnoCan and a team led by Prof. Daniel Offen, a leading researcher specializing in Neuroscience and Exosome technology at Tel Aviv University, will collaborate to develop the cell therapy based product on Prof. Offen’s work in the field. InnoCan and Ramot are collaborating on a new, revolutionary exosome-based technology that targets both central nervous system (CNS) indications and the Covid-19 Corona Virus. CBD-Loaded exosomes hold the potential to provide a highly synergistic effect of anti-inflammatory properties and help in the recovery of infected lung cells. The techology, which is expected to be administered by inhalation, will be tested on a variety of lung infections. Exosomes are small particles created when stem cells are multiplied. Exosomes can act as “homing missiles” when the cell healing properties of the exosomes are combined with the anti-inflammatory properties of CBD. Exosomes also have an important role in cell-to-cell communication, which can be beneficial to additional treatments for CNS indications such as epilepsy and Alzheimer’s Disease.Background
The world is suffering from a rapid rise in illness due to the fast growing spread of the COVID-19 pandemic. The lungs are the organ most affected by COVID-19, causing pneumonia that rapidly progresses to acute respiratory distress syndrome and can further result in respiratory failure, septic shock, multi-organ failure, and in the most severe cases death. Recent in-vivo and in-vitro studies have demonstrated that exosomes derived from mesenchymal stem cells (MSC) can promote regeneration and improve immune reaction processes in damaged tissues. Exosomes contain anti-inflammatory agents that can target inflamed organs. Prof. Offen and his team have already successfully loaded exosomes with various molecules. They have also succeeded in treating different tissue injuries in animal models, while significantly reducing inflammation and pathological impairment. To date, there have been hundreds of clinical studies using exosomes globally, demonstrating their therapeutic potential at different applications. Animal studies have also demonstrated CBD as effective in reducing lung inflammation. Based on these findings, InnoCan believes that its CLX therapy has the potential to treat the COVID-19 virus by combining CBD with exosomes, thereby creating therapeutic synergies. The suggested combination may have strong synergetic effects, thereby increasing the potential efficacy of planned treatments. Prof. Dani Offen, of the Sackler School of Medicine and Sagol School of Neuroscience said, “I am pleased to work with the InnoCan team on this exciting CLX development project. We are facing a challenging time, and I believe our unique approach holds a promise to offer a treatment for COVID-19, pneumonia and perhaps for other lung inflammations as well.” Iris Bincovich, CEO of InnoCan’s CEO, also commented, “COVID-19 has quickly become one of the largest challenges in healthcare today. With the development of CLX, we are creating a new treatment, to join the global mission to combat the effects of COVID-19. We are determined to make a difference as quickly as possible to assist patients worldwide.” Keren Primor Cohen, CEO of Ramot at Tel Aviv University, summarized, “We hope that this collaboration with Innocan will assist in transforming Prof. Offen’s promising technology into a real treatment for the global threat of COVID-19”. Featured image: Prof. Daniel Offen (photo: Jonathan Blum)TAU Scientist Awarded U.S. Patent for Novel Coronavirus Vaccine Design
The patent, approved in March, covers a vaccine that targets the most vulnerable point in a coronavirus’s structure, through which it penetrates human cells
Researchers worldwide are racing at breakneck speed to develop potential vaccines and drugs to fight the novel coronavirus, SARS-Cov-2. Now, the United States Patent and Trademark Office (USPTO) has granted a patent to Tel Aviv University’s Prof. Jonathan Gershoni of the School of Molecular Cell Biology and Biotechnology at TAU’s George S. Wise Faculty of Life Sciences for his innovative vaccine design for the corona family of viruses.
The vaccine targets the novel coronavirus’s Achilles’ heel, its Receptor Binding Motif (RBM), a critical structure that enables the virus to bind to and infect a target cell.
According to Prof. Gershoni, the vaccine would reconstruct the coronavirus’s RBM, a tiny feature of its “spike” protein. Though the virus uses many different proteins to replicate and invade cells, the “spike” protein is the major surface protein that it uses to bind to a receptor — another protein that acts like a doorway into a human cell. After the spike protein binds to the human cell receptor, the viral membrane fuses with the human cell membrane, allowing the genome of the virus to enter human cells and begin infection.
“We have been working on coronaviruses for the last 15 years, developing a method of reconstructing and reconstituting the RBM feature of the spike protein in SARS CoV and subsequently in MERS CoV,” explains Prof. Gershoni. “The moment the genome of the new virus was published in early January 2020, we began the process of reconstituting the RBM of SARS CoV2, the virus that causes COVID-19, and expect to have a reconstituted RBM of the new virus soon. This will be the basis for a new vaccine, which could be ready for use within a year to a year and a half.”
The spike protein is quite large, containing about 1,200 amino acids. Some researchers have limited their research to a region of the spike known as the receptor binding domain (RBD) that comprises some 200 amino acids. However, the problem is that these relatively large areas have a variety of targets, and the immune system produces antibodies for all of them indiscriminately – reducing the effectiveness of a potential vaccine.
The RBM, a highly complex three dimensional structure, is only 50 amino acids long. Functionally reconstituting such a structure would be very challenging, but it would be an extremely effective basis of a vaccine, says Prof. Gershoni.
“The smaller the target and the focus of the attack, the greater the effectiveness of the vaccine,” he adds. “The virus takes far-reaching measures to hide its RBM from the human immune system, but the best way to ‘win the war’ is to develop a vaccine that specifically targets the virus’s RBM.”
Prof. Gershoni’s team has completed their initial steps toward reconstituting the new SARS CoV2’s RBM. The reconstitution of the new SARS CoV2’s RBM and its use as a basis for a new vaccine is covered by an additional pending patent application, filed by Ramot, TAU’s technology transfer arm, to the USPTO.
“Now that we have received serum samples we should be able to isolate RBM-based vaccine candidates in the next month or two,” concludes Prof. Gershoni. “The discovery and production of a functional RBM for the new coronavirus is fundamental and critical for the production of the vaccine we propose.
“Our successful isolation and reconstitution of such a functional RBM will allow the industry to incorporate it into a vaccine, which will be produced by a pharmaceutical company. Development of such an RBM-based vaccine should take months and then would need to be tested in Phase 1, 2 and 3 clinical trials which would then take up to a year.”
Donated Equipment Aids in Urgent Coronavirus Research
Shmunis family gift ramps up the scientific capabilities of the School of Molecular Cell Biology and Biotechnology.
Tel Aviv University Sets Up Emergency Lab to Expand COVID-19 Testing
specialized lab, run by TAU researchers and graduate students, was built in 3 days
University has built an emergency COVID-19 testing lab, which will allow Israel to perform an additional 2,000 coronavirus tests per day. The new facility was born virtually overnight of the interdisciplinary efforts of TAU researchers, graduate students and management staff of the Sackler Faculty of Medicine and the George S. Wise Faculty of Life Sciences. Construction for the lab began on Tuesday, March 24th, at 7 a.m., and was completed Friday, March 27th, with engineers, construction workers, professors and graduate students working around the clock. A Health Ministry official reviewed the lab to ensure that it meets health and safety protocols before commencing operations. “We realized immediately how critical testing was and how we at the University could contribute to Israel’s diagnostic landscape,” explains Prof. Ariel Munitz of Sackler’s Faculty of Medicine, who spearheaded the establishment of a testing lab on campus. “It was not an easy decision. It was unclear whether the Health Ministry would approve, and we did not know exactly what the protocol was or what was required – but we knew we needed to act.” Getting ready to perform 2,000 coronavirus tests per day
“We all understood that there was a national crisis at hand, and our first thought was how to help and contribute – we have put all other considerations aside,” adds Prof. Eran Bacharach of the School of Molecular Cell Biology and Biotechnology, Wise Faculty of Life Sciences, who is in charge of the TAU BSL2+ facility dedicated to studies of viruses and bacteria.
Prof. Bacharach also helped coordinate a TAU volunteer initiative currently underway at Israeli hospitals. “A week ago we had to convince laboratories to accept our volunteers, but today labs are approaching us.”
As a result of the TAU volunteer initiative, some 170 student volunteers are currently embedded in 12 laboratories in hospitals, including Tel Aviv Sourasky Medical Center (Ichilov Hospital), Shamir Medical Center (Assaf Harofeh), Rambam Health Care Campus, Soroka Medical Center, and HMOs across Israel.
Getting ready to perform 2,000 coronavirus tests per day
“We all understood that there was a national crisis at hand, and our first thought was how to help and contribute – we have put all other considerations aside,” adds Prof. Eran Bacharach of the School of Molecular Cell Biology and Biotechnology, Wise Faculty of Life Sciences, who is in charge of the TAU BSL2+ facility dedicated to studies of viruses and bacteria.
Prof. Bacharach also helped coordinate a TAU volunteer initiative currently underway at Israeli hospitals. “A week ago we had to convince laboratories to accept our volunteers, but today labs are approaching us.”
As a result of the TAU volunteer initiative, some 170 student volunteers are currently embedded in 12 laboratories in hospitals, including Tel Aviv Sourasky Medical Center (Ichilov Hospital), Shamir Medical Center (Assaf Harofeh), Rambam Health Care Campus, Soroka Medical Center, and HMOs across Israel.
.jpg) TAU volunteers at Tel Aviv Sourasky Medical Center (Ichilov Hospital)
But after technicians at the Sheba Medical Center’s laboratory were quarantined as a result of exposure to COVID-19, TAU recognized an opportunity to contribute even further to Israel’s coronavirus efforts by performing public testing.
“We contacted University management, who got involved immediately and quickly approved an emergency budget for the project,” says Prof. Munitz. “The safety of the team operating the lab is and remains our highest priority, and we are taking every necessary precaution in strict alignment with Health Ministry regulations. The goal was to design a lab that could process up to 2,000 tests a day, and we have accomplished it.”
“Usually, setting up a lab takes 4-6 months,” concludes Ofer Lugassi, VP of Engineering and Maintenance at TAU. “To do so within a few days required the extraordinary efforts of project partners working around the clock and adopting innovative ideas, including architect Daniel Zarchi who designed the lab. Without the full mobilization of the entire team, it would never have happened. We learned and solved everything ‘on the go’: from building a new ceiling, something we didn’t anticipate we would need to do, to installing a complex air filtration system that normally takes about a month to set up. Everything was done overnight.”
TAU volunteers at Tel Aviv Sourasky Medical Center (Ichilov Hospital)
But after technicians at the Sheba Medical Center’s laboratory were quarantined as a result of exposure to COVID-19, TAU recognized an opportunity to contribute even further to Israel’s coronavirus efforts by performing public testing.
“We contacted University management, who got involved immediately and quickly approved an emergency budget for the project,” says Prof. Munitz. “The safety of the team operating the lab is and remains our highest priority, and we are taking every necessary precaution in strict alignment with Health Ministry regulations. The goal was to design a lab that could process up to 2,000 tests a day, and we have accomplished it.”
“Usually, setting up a lab takes 4-6 months,” concludes Ofer Lugassi, VP of Engineering and Maintenance at TAU. “To do so within a few days required the extraordinary efforts of project partners working around the clock and adopting innovative ideas, including architect Daniel Zarchi who designed the lab. Without the full mobilization of the entire team, it would never have happened. We learned and solved everything ‘on the go’: from building a new ceiling, something we didn’t anticipate we would need to do, to installing a complex air filtration system that normally takes about a month to set up. Everything was done overnight.”
 TAU researcher checking the lab facilities
Featured image: Prof. Ariel Munitz
TAU researcher checking the lab facilities
Featured image: Prof. Ariel Munitz
Live Webinar: Corona Virus crisis and the future of Disaster Management
Insights into the global shifts from a medical, ethical, economic, and mental health perspective – what lies ahead?
Date: Monday, April 6 Time: 11:00 AM EST / 16:00 PM CET / 18:00 PM IL
Join Tel Aviv University’s emergency and disaster faculty and its assessment of the current corona crisis. This interdisciplinary panel of experts will offer insights into the global shifts taking place from a medical, ethical, economic, and mental health perspective and what lies ahead.
The webinar will be moderated by : Dr. Bruria Adini, Head of the Emergency & Disaster Management Department, School of Public Health, Sackler Faculty of Medicine.
Panelists: Dr. Yoav Yehezkeli, Disaster management of biological hazards Prof. Michael Alkan, Infectious diseases & humanitarian aid Prof. Nava Haruvi, Economic aspects Dr. Zohar Rubinshtein – Resilience and mental health Mr. Gili Shenhar, Risk communication
For more information you may refer to our FB event page.
TAU researcher launches urgent push to beat corona
Dr. Natalia Freund is analyzing immunity of Israelis who have recovered from the virus.
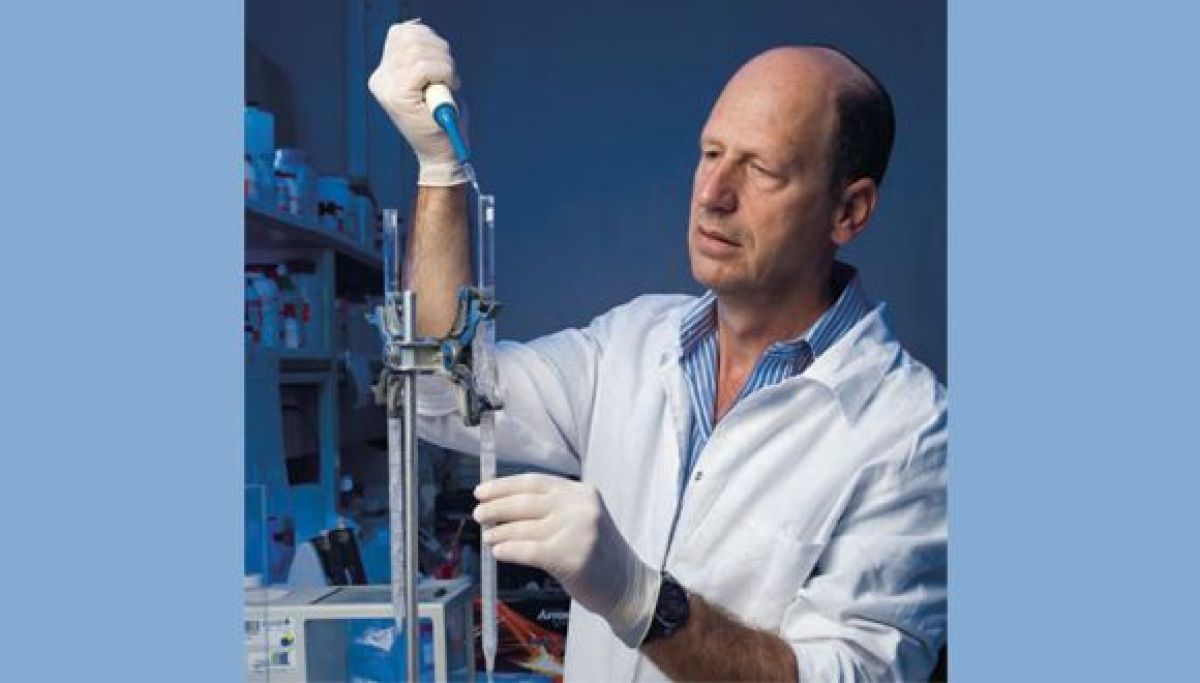
TAU researcher Dr. Natalia Freund and her team have abandoned their everyday work of isolating antibodies for HIV and other infectious diseases to urgently fight and treat COVID-19, the new coronavirus. The highly contagious disease has been declared a global pandemic by the World Health Organization, with almost 200,000 cases worldwide at press time.
Freund, a Senior Lecturer in the Department of Microbiology and Immunology at the Sackler Faculty of Medicine, will analyze blood samples from Israelis who have recovered from COVID-19 (eleven at press time). Working with graduate student Michael Mordekovich, she will use cutting-edge technology to isolate and extract special cells that produce antibodies following infection and immunize us against the virus. From these cells, she will isolate antibodies against the virus, produce them in her lab and test them for viral inhibition.
Hope for a vaccine
Freund is hopeful that within a few weeks her team will generate an antibody that will be ready for preclinical trials. The anticipated result is a treatment for COVID-19 patients and a candidate for the development of a vaccine, “although these would be ready in a best-case scenario months down the line,” said Dr. Freund.

Dr. Natalia Freund, testing to beat the coronavirus
In attempts to stem the outbreak as soon as possible, she is working intensively with colleagues at TAU as well as at the Chaim Sheba Medical Center (Tel Hashomer Hospital), Tel Aviv Sourasky Medical Center (Ichilov Hospital), Bar-Ilan University and the Institute for Biological Research.
Aside from Dr. Freund, several more scientists at TAU are working on various aspects of COVID-19 in a campus-wide effort to better understand and overcome the virus.
What’s more important? Privacy vs. public health
Experts from Tel Aviv University answer questions about the coronavirus crisis.
On Saturday, March 14, Israel’s Prime Minister, Benjamin Netanyahu stated that the government intends to use various digital tools, the kind that have so far been used in the fight against terrorism, for the purpose of monitoring the coronavirus. His remarks remained vague and were not accompanied by detailed explanations, which raised many questions for citizens.
On the one hand, radical measures are being taken around the world to try to eradicate the coronavirus, including increased surveillance and tracking measures, in accordance with WHO recommendations. Apps and features that were previously controversial are being hailed as lifesaving. On the other hand, do public health considerations override an individual’s right to privacy? Is there a precedent for the state to surveil citizens who are not suspected of any crime? What will be done with this private information? Who will have access to it? We asked experts to shed some light on this.
Can your phone serve as your handcuffs?
On Saturday, Israel’s Prime Minister announced that among other measures being considered, there will be use of “digital tools, as done in Taiwan.” Prof. Itzhak Ben-Israel, head of the Security Studies Program at the School of Political Science, Government & Political Affairs and also of the Yuval Ne’eman workshop for Science, Technology & Security and Blavatnik Interdisciplinary Cyber Research Center said, “There are many options for this kind of surveillance. The simplest of them is to use the cellphone location function to make sure that the people who are quarantined at home aren’t leaving the house. Another option is to use the same location function to follow the path of someone who might be carrying the virus to see where they’ve been. This is a more intrusive option in terms of privacy. There are of course even more intrusive options, ‘Big Brother’ style. For example, it’s possible to track the ‘suspect’ who might be infected with the disease via the contents of their e-mail or social media, to find people the ‘suspect’ has been in touch with in recent days. In Taiwan, meanwhile, they’ve used the most minimal of the options I’ve mentioned: the use of the location function (as a kind of electronic handcuff).”
The concern: an irreparable violation of individual rights
“Israel’s Prime Minister didn’t elaborate on what measures would be taken, who would be affected by conducting the surveillance, and what legal framework would be used,” says Prof. Michael Birnhack, Deputy Dean of Research at the Buchmann Faculty of Law and also a researcher at the Balavatnik Interdisciplinary Cyber Researcher Center. “The state now has a number of legal tools to monitor people in various contexts, but there is no context that fits well with a general health emergency, such as the one we are in right now.
“Indeed, the emergency is severe, and Israel and many other countries have no prior experience in dealing with this kind of epidemic, but the right to privacy, like all human rights, is particularly important and is tested in times of crisis and emergency. A populist approach presents the situation as a dichotomy in which we must choose between public health and privacy. This is a false and misleading dichotomy. The democratic approach seeks to balance and, where possible, achieve both goals at once.
“The concern is that curtailing of rights will be difficult to fix, and emergency arrangements will remain with us long after the coronavirus disappears. To prevent such harm, the health system needs to be precisely defined. According to its needs, different tools available to the state can be examined, in order to find the course of action that last violates privacy (‘proportionality’ in legal terms).
“I can characterize some of these needs: First, the patients. They need the best care, and we all have an interest in reducing further infection. The patients’ privacy is compromised by the hospitalization. No additional follow-up measures are needed for them.
“Second, those isolated at home – the interest here is to make sure they maintain isolation lest they infect others. But here, the social solidarity, backed by the law that determines the isolation breach as a criminal offense, the ability to report someone, and the enforcement of the Ministry of Health backed by the police – are sufficient. Geolocation of people who are isolated won’t be effective. A person who wants to violate isolation will simply leave the mobile phone at home.
“Third, reconstructing the ‘path of infection’ for those who are ill. As part of the epidemiological investigation, not all patients remember where they were every hour from the 14 days prior to identifying their disease. Cellular data can help. But here, you don’t need the law. It’s enough to ask for their consent and, in my estimation, everyone will agree to give up their location data, to minimize the harm they’ve caused unintentionally.
“And fourth, locating those who have been exposed to a verified patient. Here, you need to be informed. Now, the Ministry of Health is publicizing the patients’ ‘path of infection’, but presumably the information does not reach everyone who was in the wrong place at the wrong time. Cellphone surveillance can locate them. This is where the idea of ’privacy by design’ comes into the picture. One way is that cellular companies transmit information to the state. This is a bad, disproportionate way. The goal is not to collect location information, but to inform citizens. So, the flow of information has to be reversed, so that the state asks cellular companies to contact those who were in a certain place at a certain time. The details are important, of course, and should be formulated in an integrated engineering-organizational-legal process,” concludes Prof. Birnhack.
In conclusion, responsibility seems to ultimately fall on everyone in society. It’s our responsibility to demonstrate social solidarity, to obey the instructions of official health agencies so as not to infect others, and help as much as possible those in our community who are afraid or are at higher risk. It’s also our responsibility to ask questions and not take for granted fundamental rights. It seems that balancing these two approaches will allow us to successfully overcome this crisis.
Can blood pressure in your twenties cause cognitive decline in your fifties?
TAU and Northwestern University study proves treatment for high blood pressure must begin decades earlier than it does now.
High blood pressure, or hypertension, affects everything from your arteries to your kidneys, from eyesight to sexual function. Among older adults, high blood pressure is also associated with cognitive decline as a result of interrupted blood flow to the brain, as well as strokes, heart attacks and impaired mobility.
A new Northwestern University–Tel Aviv University study has revealed that subjects who experienced relatively high blood pressure during young adulthood also experienced significant declines in cognitive function and gait in midlife (approximately 56 years old). The study cohort included about 200 young adults with an average age of 24 at the beginning of the study.
The research was led by Prof. Farzaneh A. Sorond and Dr. Simin Mahinrad of Northwestern University’s Department of Neurology and Prof. Jeffrey Hausdorff of TAU’s Sackler Faculty of Medicine, TAU’s Sagol School of Neuroscience and Tel Aviv Medical Center’s Center for the Study of Movement, Cognition, and Mobility at the Neurological Institute. The study was published in the American Heart Association’s journal Circulation on November 21, 2019.
Thirty years of data
“We find that the deleterious effects of elevated blood pressure on brain structure and function begin in early adulthood. This demonstrates the need for preventive measures of high blood pressure even at this early age,” explains Prof. Hausdorff. “We know that poor gait and cognitive function among older adults are associated with and predict multiple adverse health outcomes like cognitive decline, dementia, falls and death. Our study shows that the time to treat high blood pressure and to minimize future changes in gait and cognition is much earlier — decades earlier — than previously thought.”
In addition, the study suggests that gait impairment may be an earlier hallmark of hypertensive brain injury than cognitive deficits.
For the study, the researchers assessed the blood pressure, gait and cognition of 191 participants from the Coronary Artery Risk Development in Young Adults study, a community-based cohort of young individuals followed over 30 years. In the last year of follow-up, gait was assessed using an instrumented gait mat; cognitive function was evaluated using neuropsychological tests; and the level of white matter intensity in the brain, a symptom of cardiovascular disease, was measured using MRIs. The impact of cumulative levels of high blood pressure was found to be independent of other vascular risk factors over the same 30-year period.
High pressure leads to smaller steps
“Higher cumulative blood pressure was associated with slower walking speed, smaller step length and higher gait variability,” Prof. Hausdorff says. “Higher cumulative blood pressure was also associated with lower cognitive performance in the executive, memory and global domains.”
“Our takeaway is this: Even in young adults, blood pressure has significant implications, even at levels below the ‘hypertension’ threshold, and is important to assess and modify for future cognitive function and mobility,” Prof. Hausdorff concludes.