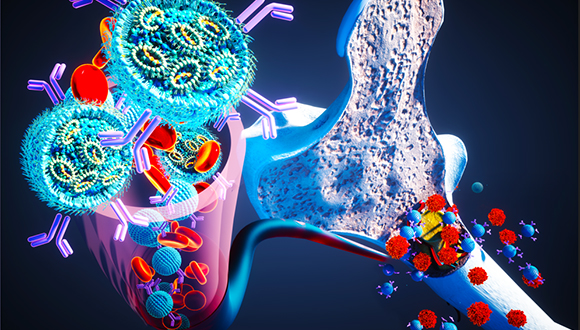
Are We Close to Ending Alzheimer’s Memory Loss?
TAU Researchers Successfully Prevent Memory Deterioration in Alzheimer’s in an Animal Model.
In 2022, a team of researchers from the laboratory of Prof. Inna Slutsky from the Faculty of Medical & Health Sciences and the Sagol School of Neuroscience at TAU uncovered a pathological brain phenomenon in an animal model that precedes the first appearance of Alzheimer’s disease symptoms by many years. This is an increased activity in the hippocampus during the states of anesthesia and sleep, which results from damage to the mechanism that stabilizes the neural network.
Breakthrough in Alzheimer’s Study
In the current study published in Nature Communications, Prof. Slutsky’s laboratory team, in collaboration with the Safra Center for Neuroscience at the Hebrew University, found that suppression of neuronal activity in a small nucleus in a specific area of the thalamus (which regulates sleep states) caused a decrease in pathological activity in the hippocampus and prevented the deterioration of the memory in Alzheimer’s in an animal model. The researchers hope that their research will speed up the start of clinical trials in humans, lead to progress in the fields of early detection and prevention of the onset of dementia symptoms in Alzheimer’s disease, and in the field of treating cognitive impairments caused by surgery (POCD – Postoperative Cognitive Dysfunction).

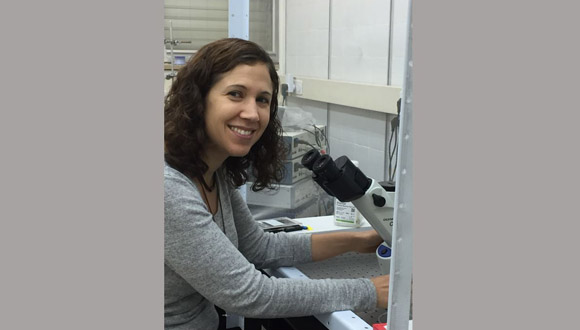
Doctoral Student Shiri Shoob
“As early as 10-20 years before the appearance of the familiar symptoms of memory impairment and cognitive decline, physiological changes slowly and gradually occur within the patients’ brains,” explains the doctoral student who led the study, Shiri Shoob. “There is an accumulation of amyloid-beta deposits and abnormal accumulations of tau protein, a decrease in the volume of the hippocampus, and more. Moreover, about 30% of the people who were found to have a pathology typical of Alzheimer’s disease at postmortem did not develop the typical symptoms of the disease during their lifetime. It seems, then, that the brain has an, admittedly limited, ability to protect itself from the damage of the disease.”
Uncovering Alzheimer’s Protective Mechanisms
The research focused on finding those protective mechanisms that the brain has against the damage from the disease. The researchers found that during sleep – and especially during sleep as a result of general anesthesia – the early symptoms of Alzheimer’s disease, which appear many years before the symptoms of dementia, could be more easily identified. Prof. Inna Slutsky: “Anesthesia reveals pathophysiology in the brain activity in the animal model. We think that there are mechanisms that compensate for that same pathology while awake and thus prolong the pre-symptomatic period of the disease”.

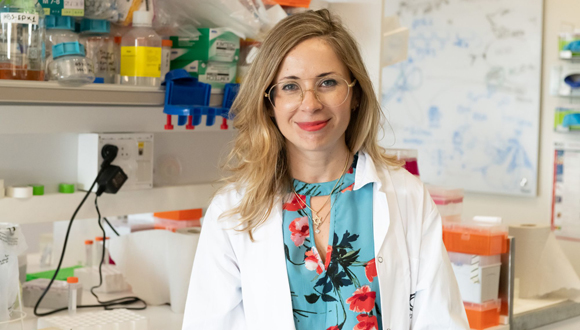
Prof. Inna Slutsky
The researchers identified hyperactivity in the hippocampus – “silent seizures,” which look like an epileptic seizure in terms of brain activity, but do not appear externally – in in an animal model of Alzheimer’s disease.This, compared to the reduced activity in the healthy hippocampus during sleep and anesthesia. To examine potential treatment and prevention measures, the researchers tried a variety of methods, but mainly focused on deep brain stimulation (DBS) using electrical signals to the nucleus reuniens – a small nucleus in the brain that connects the affected hippocampus and the thalamus, which is responsible for sleep regulation.
“When we tried to stimulate the nucleus reuniens at high frequencies, as is done in the treatment of Parkinson’s, for example, we found that it worsened the damage to the hippocampus and the silent epileptic seizures,” said Shoob, “only after changing the stimulation pattern to a lower frequency were we able to suppress the seizures and prevent cognitive impairment. We showed that the nucleus reuniens could completely control these seizures. We could increase or decrease the seizures by stimulating it”.
Decoding Alzheimer’s
Prof. Slutsky adds: “Epidemiological studies indicate a link between aging and a phenomenon called POCD – cognitive problems that arise after surgery under general anesthesia. In young people, the symptoms usually pass very quickly, but in older people, the chance of cognitive impairment increases and it may last a long time. Our research indicates a potential mechanism underlying the phenomenon. We found that suppressing the thalamic nucleus reuniens – by pharmacological or electrical means – successfully prevented both pathological activity in the hippocampus during anesthesia and cognitive impairment following anesthesia.
In addition, we identified a relationship between certain pathological activity in the hippocampus during anesthesia in the presymptomatic phase of Alzheimer’s to memory problems in a more advanced stage of the disease. This indicates a potential for predicting the disease in the dormant state, before the onset of cognitive decline”.
The leader of the study, Shiri Shoob, added: “We saw that no matter what means we used, when we inhibited the neural activity in the nucleus, we also measured a decrease in the pathological activity in the hippocampus during anesthesia”.
The research was led by PhD student Shiri Shoob, with the participation of Nadav Buchbinder, PhD student Ortal Shinikamin, Halit Baeloha, Dr. Tomer Langberg, Dr. Daniel Zarhin, Dr. Ilana Shapira and Dr. Gabriella Braun from Prof. Inna Slutsky’s lab and in collaboration with Dr. Naomi Habib and Or Gold from the Hebrew University.